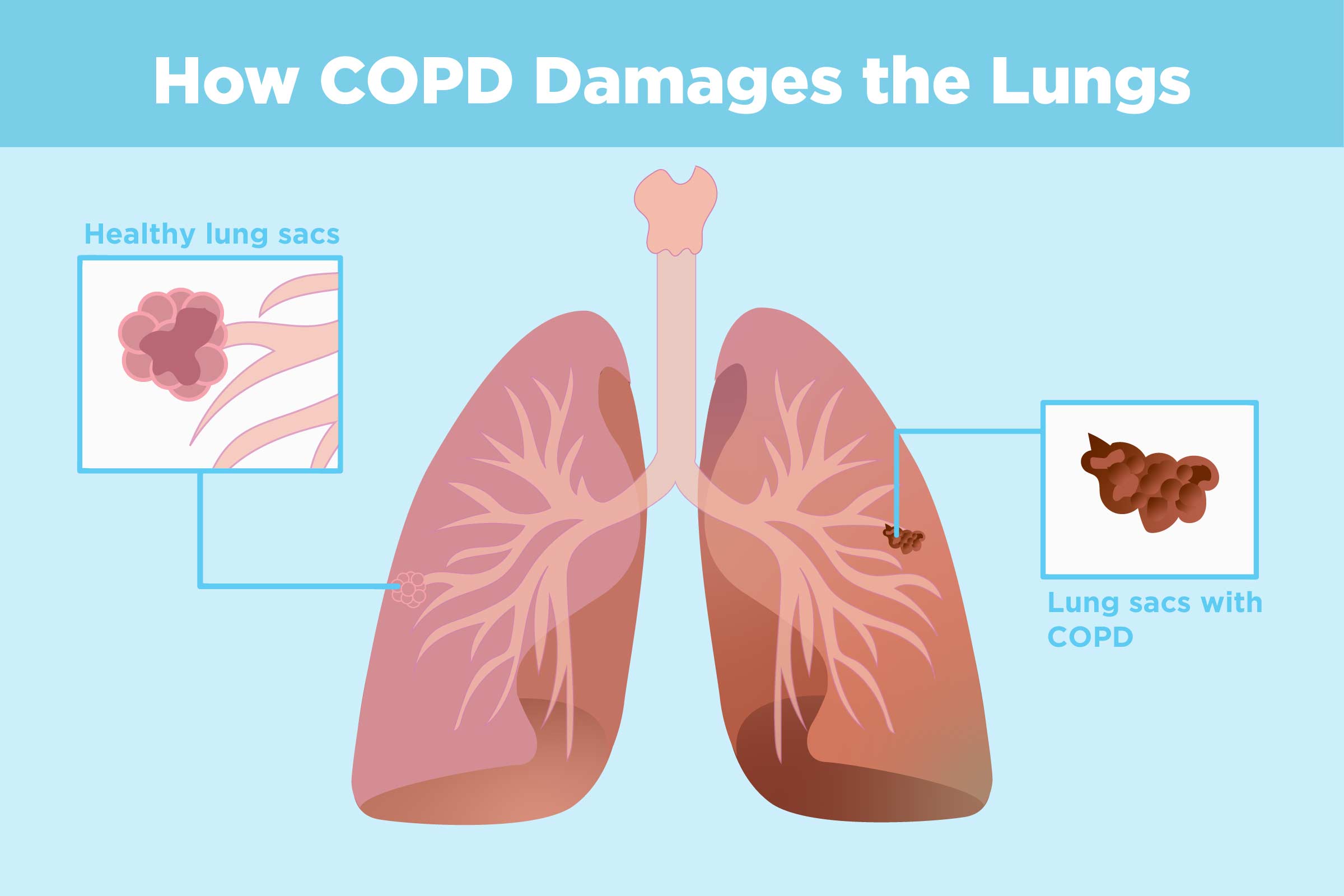
Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases. It makes it difficult to breathe. There are two main forms of COPD:
- Chronic bronchitis, defined by a long-term cough with mucus
- Emphysema, defined by destruction of the lungs over time
Most people with COPD have a combination of both conditions.
Symptoms
- Cough with mucus
- Shortness of breath (dyspnea) that gets worse with mild activity
- Fatigue
- Frequent respiratory infections
- Wheezing
In order to establish disability due to COPD, it is important to get medical treatment and to keep your doctor aware of the symptoms you’re experiencing and how those symptoms are affecting your life, including your ability to work, to go to school, and to perform activities of daily living. Keeping a journal of your symptoms and/or attacks or episodes is helpful. United Disability Lawyers Group knows the right questions to ask and how to best present your case to establish disability based on COPD and any other impairments you may have.
Signs and tests
The best test for COPD is a simple lung function test called spirometry. This involves blowing out as hard as one can into a small machine that tests lung capacity. The test can be interpreted immediately and does not involve exercising, drawing blood, or exposure to radiation. Blood tests may also be helpful.
To read more about COPD, see: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001153/
Social Security’s Listing regarding COPD and other pulmonary disorders:
3.01 Category of Impairments, Respiratory System
http://www.ssa.gov/disability/professionals/bluebook/3.00-Respiratory-Adult.htm
3.02 Chronic pulmonary insufficiency
A. Chronic obstructive pulmonary disease due to any cause, with the FEV1 equal to or less than the values specified in table I corresponding to the person’s height without shoes. (In cases of marked spinal deformity, see 3.00E.);
Table I
| Height without Shoes (centimeters) |
Height without Shoes (inches) | FEV1Equal to or less than (L,BTPS) |
| 154 or less | 60 or less | 1.05 |
| 155-160 | 61-63 | 1.15 |
| 161-165 | 64-65 | 1.25 |
| 166-170 | 66-67 | 1.35 |
| 171-175 | 68-69 | 1.45 |
| 176-180 | 70-71 | 1.55 |
| 181 or more | 72 or more | 1.65 |
or
B. Chronic restrictive ventilatory disease, due to any cause, with the FVC equal to or less than the values specified in Table II corresponding to the person’s height without shoes. (In cases of marked spinal deformity, see 3.00E.);
Table II
| Height without Shoes (centimeters) |
Height without Shoes (inches) |
FVC Equal to or less than (L,BTPS) |
| 154 or less | 60 or less | 1.25 |
| 155-160 | 61-63 | 1.35 |
| 161-165 | 64-65 | 1.45/td> |
| 166-170 | 66-67 | 1.55 |
| 171-175 | 68-69 | 1.65 |
| 176-180 | 70-71 | 1.75 |
| 181 or more | 72 or more | 1.85 |
or
C. Chronic impairment of gas exchange due to clinically documented pulmonary disease. With:
1. Single breath DLCO (see 3.00Fl) less than 10.5 ml/min/mm Hg or less than 40 percent of the predicted normal value. (Predicted values must either be based on data obtained at the test site or published values from a laboratory using the same technique as the test site. The source of the predicted values should be reported. If they are not published, they should be submitted in the form of a table or nomogram); or
2. Arterial blood gas values of PO2 and simultaneously determined PCO2 measured while at rest (breathing room air, awake and sitting or standing) in a clinically stable condition on at least two occasions, three or more weeks apart within a 6-month period, equal to or, less then the values specified in the applicable table III-A or III-B or III-C:
Table III-A
(Applicable at test sites less than 3,000 feet
above sea level)
| Arterial PCO2 (mm Hg) and | Arterial PO2 Equal to or Less than (mm Hg) |
| 30 or below | 65 |
| 31 . . . . . | 64 |
| 32 . . . . . | 63 |
| 33 . . . . . | 62 |
| 34 . . . . . | 61 |
| 35 . . . . . | 60 |
| 36 . . . . . | 59 |
| 37 . . . . . | 58 |
| 38 . . . . . | 57 |
| 39 . . . . . | 56 |
| 40 or above | 55 |
Table III-B
(Applicable at test sites 3,000 through 6,000 feet above sea level)
| Arterial PCO2 (mm Hg) and |
Arterial PO2 Equal to or Less than (mm Hg) |
| 30 or below | 60 |
| 31 . . …… . | 59 |
| 32 . . . . . | 58 |
| 33 . . . . . | 57 |
| 34 . . . . . | 56 |
| 35 . . . . . . | 55 |
| 36 . . . . . . | 54 |
| 37 . . . . . . | 53 |
| 38 . . . . . . | 52 |
| 39 . . . . . . | 51 |
| 40 or above | 50 |
Table III-C
(Applicable at test sites over 6,000 feet above sea level)
| Arterial PCO2 (mm Hg) and |
Arterial PO2equal to or less than (mm Hg) |
| 30 or below . | 55 |
| 31 . . . . . . . | 54 |
| 32 . . . . . . . | 53 |
| 33 . . . . . . . | 52 |
| 34 . . . . . . . | 51 |
| 35 . . . . . . . | 50 |
| 36 . . . . . . . | 49 |
| 37 . . . . . . . | 48 |
| 38 . . . . . . . | 47 |
| 39 . . . . . . . | 46 |
| 40 or above | 45 |
or
3. Arterial blood gas values of PO2 and simultaneously determined PCO2 during steady state exercise breathing room air (level of exercise equivalent to or less than 17.5 ml O2consumption/kg/min or 5 METs) equal to or less than the values specified in the applicable table III-A or III-B or III-C in 3.02 C2.
3.03 Asthma With:
A.Chronic asthmatic bronchitis. Evaluate under the criteria for chronic obstructive pulmonary disease in 3.02A;
or
B. Attacks (as defined in 3.00C), in spite of prescribed treatment and requiring physician intervention, occurring at least once every 2 months or at least six times a year. Each in-patient hospitalization for longer than 24 hours for control of asthma counts as two attacks, and an evaluation period of at least 12 consecutive months must be used to determine the frequency of attacks.
3.04 Cystic fibrosis. With:
A. An FEV1 equal to or less than the appropriate value specified in table IV corresponding to the individual’s height without shoes. (In cases of marked spinal deformity, see. 3.00E.);
or
B. Episodes of bronchitis or pneumonia or hemoptysis (more than bloodstreaked sputum) or respiratory failure (documented according to 3.00C, requiring physician intervention, occurring at least once every 2 months or at least six times a year. Each inpatient hospitalization for longer than 24 hours for treatment counts as two episodes, and an evaluation period of at least 12 consecutive months must be used to determine the frequency of episodes;
or
C. Persistent pulmonary infection accompanied by superimposed, recurrent, symptomatic episodes of increased bacterial infection occurring at least once every 6 months and requiring intravenous or nebulization antimicrobial therapy.
Table IV
(Applicable only for evaluation under
3.04A – cystic fibrosis)
| Height without Shoes (centimeters) | Height without Shoes (inches) | FEV1Equal to or less than (L,BTPS) |
| 154 or less | 60 or less | 1.45 |
| 155-159 | 61-62 | 1.55 |
| 160-164 | 63-64 | 1.65 |
| 165-169 | 65-66 | 1.75 |
| 170-174 | 67-68 | 1.85 |
| 175-179 | 69-70 | 1.95 |
| 180 or more | 71 or more | 2.05 |
3.06 Pneumoconiosis
(demonstrated by appropriate imaging techniques). Evaluate under the appropriate criteria in 3.02.
3.07 Bronchiectasis
(demonstrated by appropriate imaging techniques). With:
A. Impairment of pulmonary function due to extensive disease. Evaluate under the appropriate criteria in 3.02;
or
B. Episodes of bronchitis or pneumonia or hemoptysis (more than bloodstreaked sputum) or respiratory failure (documented according to 3.00C), requiring physician intervention, occurring at least once every 2 months or at least six times a year. Each inpatient hospitalization for longer than 24 hours for treatment counts as two episodes, and an evaluation of at least 12 consecutive months must be used to determine the frequency of episodes.
3.08 Mycobacterial, mycotic, and other chronic persistent infections of the lung
(see 3.00B). Evaluate under the appropriate criteria in 3.02.
3.09 Cor pulmonale secondary to chronic pulmonary vascular hypertension
Clinical evidence of cor pulmonale (documented according to 3.00G) with:
A. Mean pulmonary artery pressure greater than 40 mm Hg;
or
B. Arterial hypoxemia. Evaluate under the criteria in 3.02C2.
3.10 Sleep-related breathing disorders. Evaluate under 3.09 (chronic cor pulmonale), or 12.02 (organic mental disorders).
3.11 Lung transplant. Consider under a disability for 12 months following the date of surgery; thereafter, evaluate the residual impairment
To read more about the Social Security Administration’s pulmonary listings, see:
http://www.ssa.gov/disability/professionals/bluebook/3.00-Respiratory-Adult.htm